Brain-computer interfaces are opening new medical possibilities you’ll want to follow. They’re helping ALS patients restore speech and emotional connections, with implants working reliably for years. BCIs also assist stroke recovery by improving motor skills through innovative feedback systems. Advances in diagnostics, surgical precision, and AI-driven analysis are making treatments safer and more personalized. As technology progresses, ethical and security questions arise. If you keep exploring, you’ll discover how these breakthroughs could transform healthcare for many.
Key Takeaways
- BCIs are improving communication for ALS patients with up to 97% accuracy, restoring speech and emotional expression.
- Long-term stable implantable BCIs enable reliable control of devices and smart homes, enhancing independence.
- BCIs facilitate motor recovery post-stroke by promoting neural plasticity through real-time feedback and combined therapies.
- Advances in high-resolution neural monitoring and AI enhance diagnostic precision and personalized surgical interventions.
- Ethical and security challenges are being addressed to ensure safe, autonomous, and trustworthy integration of BCIs in healthcare.
Transforming Communication for ALS Patients

Brain-Computer Interfaces (BCIs) are revolutionizing communication for ALS patients by translating their brain signals into speech with remarkable accuracy and speed. UC Davis’s system achieves up to 97% accuracy, enabling patients to communicate within minutes of activation. It converts brain signals during attempted speech into text, then vocalizes it through a computer voice, helping users reconnect with family and caregivers. Johns Hopkins reports implantable BCIs that reliably control communication devices and smart home systems for months without recalibration. These BCIs can be invasive or non-invasive, affecting ease of use and training time. They aim to restore natural conversation and emotional expression, profoundly improving quality of life. As the technology advances, it offers hope for more seamless and effective communication solutions for those with severe speech impairments caused by ALS. Additionally, ongoing research into high-resolution neural recording is expected to enhance the precision and responsiveness of future BCI systems. Incorporating mindfulness techniques into BCI training protocols may further optimize user adaptation and comfort. Furthermore, advancements in AI-driven signal decoding are likely to improve the accuracy and speed of translating brain signals, making BCIs more accessible and reliable for users.
Long-Term Success of Implants in Restoring Function
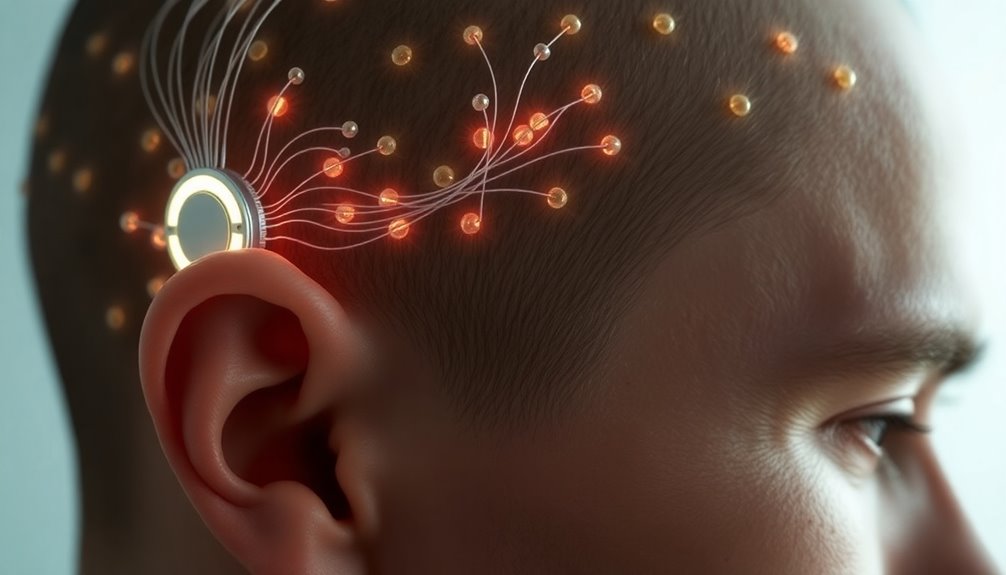
Implanted BCIs have shown impressive long-term stability and performance, making them a viable option for restoring function in patients with severe neurological impairments. In late-stage ALS patients, ECoG-based BCIs provided stable control signals and high user performance over 36 months. Although power in the high-frequency control band declined slowly, it didn’t impact device function. Electrode impedance increased until about month 5 post-implantation, then stabilized, supporting durability. The steady rise in home use shows users increasingly adopt and rely on these devices daily. Safety profiles from large trials reveal low rates of serious adverse events, with minimally invasive methods further enhancing safety. Advances in technology, materials, and implantation techniques continue to extend the longevity and reliability of these implants, highlighting the importance of durability, as long-term stability is crucial for therapeutic success. Additionally, ongoing research emphasizes the role of device maintenance and monitoring in ensuring sustained performance over time. Furthermore, dream-like experiences during long-term use may influence patient perceptions and acceptance of these technologies, underscoring the importance of understanding user experience for optimizing outcomes.
Rehabilitating Motor Skills After Stroke
Rehabilitating motor skills after stroke has seen significant advancements through the use of brain-computer interface (BCI) systems, which facilitate direct communication between the brain and external devices. BCIs provide sensory feedback of brain oscillations, helping you modulate sensorimotor rhythms intentionally. They use real-time neural activity to control external devices, promoting neural plasticity through feedback. Motor imagery-based BCIs stimulate the motor cortex, improving cortical connections and restoring function. Closed-loop systems ensure continuous interaction, adapting feedback to support learning. Studies show BCI therapy enhances upper limb motor function and triggers lasting neurological changes. Both non-invasive and invasive BCIs, combined with technologies like VR or FES, optimize recovery. Clinical trials and meta-analyses confirm BCI’s promising role in improving motor impairment scores, like those measured by the Fugl-Meyer scale. Emphasizing the importance of neural plasticity, these innovations continue to expand the possibilities for stroke rehabilitation. Additionally, integrating personalized feedback mechanisms can further enhance motor recovery outcomes by tailoring interventions to individual neural responses. Moreover, leveraging insights from anatomical and physiological studies can guide the development of more effective BCI systems for personalized therapy, fostering a deeper understanding of neural mechanisms. Recognizing the significance of sensory feedback in neural adaptation can lead to even more targeted and effective rehabilitation strategies.
Enhancing Diagnostic and Surgical Precision

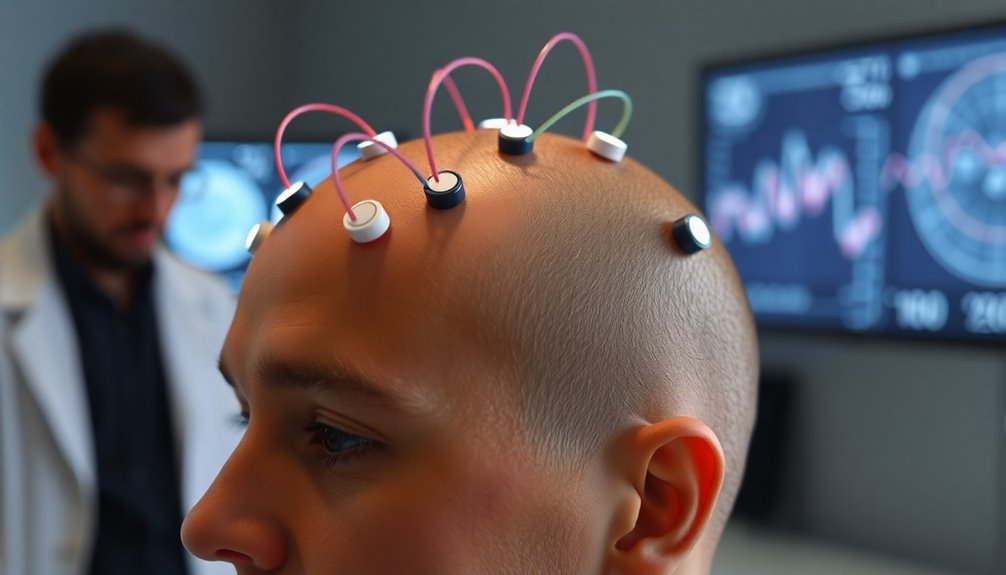
How can emerging technologies enhance the accuracy of neurological diagnoses and surgical procedures? Brain-Computer Interfaces (BCIs) are advancing diagnostics by providing high-resolution neural readings through electrocorticography, especially with invasive BCIs that offer superior signal quality. These detailed signals improve the detection of neurological disorders like Parkinson’s disease. In surgery, high-density BCIs such as the Layer 7 Cortical Interface enable real-time neural monitoring with submillimeter precision, guiding safer, more accurate procedures. When combined with AI, BCIs automate image segmentation and provide real-time data analysis, reducing human error. This integration of neural data processing is opening new avenues for personalized and adaptive treatment plans. This synergy allows for closed-loop systems that adapt during surgery, improving outcomes. Additionally, ongoing research and development in neural signal processing are expanding the potential applications of BCIs in clinical settings. For instance, advances in signal decoding algorithms are enhancing the interpretability of neural data, leading to more precise interventions. Moreover, innovations in biomedical engineering are facilitating the development of more biocompatible and durable implants, further advancing BCI technology. Furthermore, the integration of machine learning techniques is optimizing the accuracy of neural signal interpretation, enabling more reliable diagnostics. Overall, these innovations refine diagnostic accuracy and surgical precision, leading to better patient care and safer procedures.
Navigating Ethical and Technological Frontiers

Exploring the ethical and technological frontiers of Brain-Computer Interfaces raises critical questions about how we balance innovation with responsibility. You must consider cognitive liberty, as BCIs risk unwarranted intrusion into mental processes and neural data, threatening mental privacy by exposing thoughts, emotions, and intentions. Protecting user autonomy is crucial, especially to prevent external manipulation or coercion in workplaces or healthcare. Cybersecurity challenges include data breaches, thought manipulation, and the need for encryption and regular security audits, with current standards often lacking specificity. Societal issues, like accessibility, cost barriers, and potential discrimination, threaten to deepen inequalities. Legally, inconsistent oversight and liability uncertainties complicate regulation. To navigate these frontiers, developing ethical guidelines, clear data ownership policies, and fostering global collaboration are essential for responsible BCI advancement. Additionally, understanding the importance of expert voice actors in communicating complex topics can help inform public discourse and build trust in emerging technologies. Recognizing the influence of psychological factors related to narcissistic traits can also aid in shaping ethical considerations around user mental health and autonomy. Furthermore, addressing technological vulnerabilities is vital to ensure the integrity and safety of BCI systems against emerging cyber threats.
Frequently Asked Questions
What Are the Costs Associated With BCI Technology and Its Accessibility?
You wonder about BCI costs and accessibility. Initially, noninvasive systems range from $5,000 to $10,000, with ongoing expenses for support and upgrades. Emerging low-cost platforms aim to cut hardware prices below $250. Access depends on who covers the costs—insurance, providers, or patients—shaped by policies and socioeconomic factors. As the market grows, affordability and equitable distribution will be essential, but regulatory and infrastructure challenges may influence widespread adoption.
How Do BCIS Adapt to Individual Brain Signal Variability Over Time?
Imagine your brain signals as a shifting river, unpredictable and ever-changing. You see, BCIs adapt by using machine learning to recalibrate based on your current signals, like a captain adjusting sails to catch the wind. Transfer learning helps BCIs learn from previous experiences, reducing the need for constant retraining. By focusing on specific EEG rhythms and providing real-time feedback, they stay aligned with your unique brain patterns over time.
What Are the Potential Psychological Effects of Long-Term BCI Use?
You might experience psychological effects from long-term BCI use, such as increased anxiety or frustration if your performance doesn’t meet expectations. It can also influence your self-perception and identity, requiring mental adaptation. While BCIs have potential for mental health treatments, they could cause emotional shifts or fatigue over time. Managing motivation, session length, and emotional responses is essential to maintain your well-being and maximize benefits.
How Is Patient Data Privacy Protected in BCI Applications?
Think of your neural data as a secret map, revealing your innermost thoughts and feelings. To protect your privacy, BCI developers use strong encryption, secure storage, and strict access controls. They also make sure you give informed consent and keep data anonymized. Regulations are evolving, and transparency is key. By following privacy-by-design principles and collaborating with authorities, they aim to safeguard your mental privacy against misuse or unauthorized access.
What Regulatory Challenges Must BCIS Overcome Before Widespread Clinical Use?
You need to address regulatory challenges like fragmented laws and lack of unified standards, which complicate governance. Clear regulations must evolve to manage safety, cybersecurity, and ethical concerns, including informed consent and cognitive liberty. Ensuring robust privacy protections for neural data is essential. International cooperation is crucial to harmonize standards, while ongoing oversight should monitor device safety, data security, and ethical use, paving the way for responsible, widespread BCI clinical applications.
Conclusion
As you explore brain-computer interfaces, you’ll see they’re transforming lives. Did you know that over 85% of ALS patients using these devices regain some level of communication? These breakthroughs promise a future where restoring motor skills and improving diagnostics become routine. As technology advances, it’s essential to navigate ethical questions carefully. Embrace the potential—you’re witnessing the dawn of a new era in medicine that could change countless lives for the better.