Inflamm-aging refers to the gradual, low-grade inflammation that increases as you age, affecting your immune system and damaging tissues. This persistent inflammation involves cytokines like IL-6 and TNF-alpha, leading to issues such as heart disease, neurodegeneration, and muscle decline. Cellular changes, immune cell shifts, and signaling pathways like NF-κB fuel this process. To understand how you can counteract inflamm-aging and promote healthy aging, keep exploring these complex mechanisms.
Key Takeaways
- Inflammaging is a chronic, low-grade inflammation that increases with age, contributing to tissue damage and age-related diseases.
- Elevated cytokines like IL-6, IL-1, and TNF-alpha drive persistent inflammation in aging tissues.
- Cellular senescence and SASP secretion amplify inflammatory responses, worsening tissue deterioration.
- Immune system aging involves reduced efficacy of T and B cells, promoting inflammation and susceptibility to infections.
- Targeting senescent cells and inflammatory pathways offers potential strategies to mitigate inflammaging effects.
Understanding Inflammaging: The Basics of Aging and Inflammation
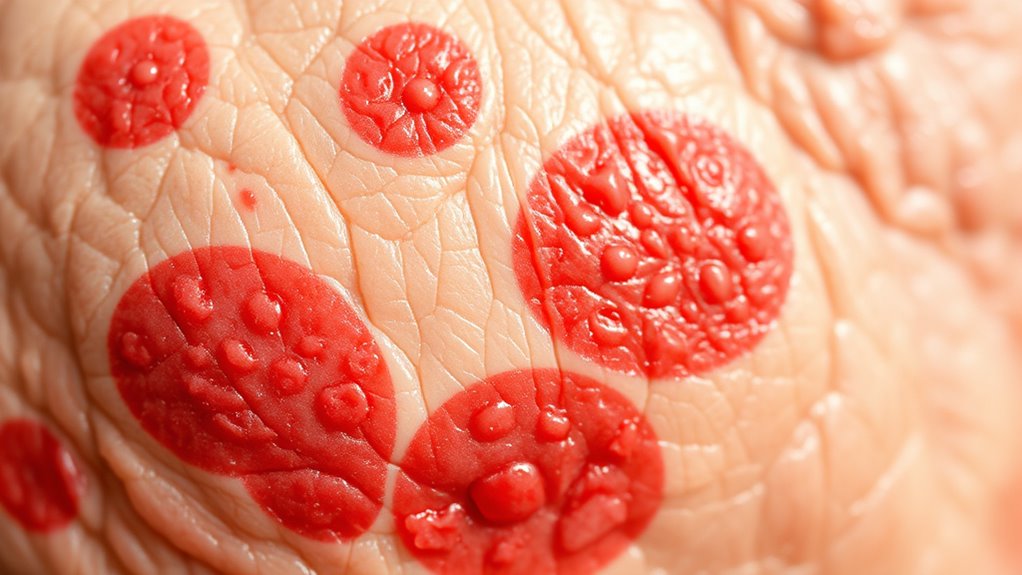
As you age, your body experiences a slow, persistent increase in inflammation, known as inflammaging. This process involves low-grade, chronic inflammation that gradually develops over time, contributing to aging and related diseases.
Inflammaging is characterized by elevated levels of inflammatory cytokines like IL-6, IL-1, and TNF-alpha, which can weaken your immune system. Chronic inflammation plays a central role in this process, leading to tissue damage and age-related decline. Additionally, the accumulation of senescent cells further exacerbates the inflammatory environment, impairing tissue repair and regeneration. Recent studies also suggest that neuroinflammation may be involved in cognitive decline associated with aging.
Elevated cytokines like IL-6, IL-1, and TNF-alpha weaken your immune system.
As you get older, your immune cells become less effective, partly because of cellular senescence and the secretion of harmful substances called SASP. immune system decline accelerates the progression of inflammaging and age-related diseases. Molecular mechanisms like inflammasome activation, oxidative stress, and mitochondrial dysfunction keep this inflammation ongoing. These pathways are often interconnected, amplifying the inflammatory response and accelerating aging. Inflammasome activation is a key driver in the process, prompting the release of inflammatory mediators that sustain inflammaging.
Lifestyle choices, such as diet and exercise, can influence inflammaging, either accelerating or helping to mitigate its effects on your aging process. Recent research emphasizes the importance of AI safety measures in monitoring and understanding the complex biological processes involved in aging, including inflammaging.
How Chronic Inflammation Impacts Different Body Systems

Chronic inflammation from inflammaging affects multiple body systems, speeding up age-related decline and increasing vulnerability to disease. It disrupts the immune response, making it harder for your body to fight infections. Resources and Tools like access to healthcare professionals can help manage and mitigate these effects. In the brain, systemic inflammaging promotes neurodegenerative diseases like Alzheimer’s by activating microglia and damaging the blood-brain barrier. Additionally, ongoing research explores cybersecurity vulnerabilities that could threaten patient data in digital health systems, emphasizing the importance of robust security measures. In the cardiovascular system, persistent low-grade inflammation contributes to atherosclerosis, raising your risk for heart disease and stroke. Musculoskeletal tissues also suffer, leading to conditions like arthritis and osteoporosis. Exploring anti-inflammatory strategies may provide avenues to reduce the impact of inflammaging on various organs. Furthermore, understanding how systemic inflammation interacts with different organs can help develop targeted interventions to slow aging processes. Moreover, advances in AI in Education could support personalized health management and patient education, improving outcomes in aging populations.
Cellular Changes Driving Inflammaging
As you age, most cells become senescent, releasing pro-inflammatory factors that fuel tissue damage. These changes also alter immune cell functions, leading to increased inflammation and impaired immune responses. Understanding how cellular senescence and immune alterations drive inflammaging can help identify strategies to mitigate age-related inflammation. Additionally, the accumulation of damaged cellular components can further exacerbate inflammatory responses, contributing to the aging process. Recent studies highlight the role of cellular debris clearance in reducing inflammaging and promoting healthier aging. Furthermore, advancements in understanding cellular senescence have opened avenues for targeted therapies to combat chronic inflammation associated with aging, especially by exploring the immune system’s role in managing cellular waste. Recognizing the impact of zodiac sign compatibility on health behaviors may also provide insights into personalized approaches for aging and inflammation management.
Cellular Senescence Effects
Cellular senescence plays a key role in driving inflammaging by causing cells to stop dividing and release inflammatory factors collectively known as SASP. These inflammatory factors include cytokines like IL-6, IL-1β, and TNF-α, which promote systemic inflammation. As you age, more cells become senescent, increasing SASP secretion and fueling chronic low-grade inflammation. This buildup leads to tissue damage and decline in function. Understanding cellular senescence can help in developing targeted therapies to reduce inflammaging and improve health span. The process of cellular aging involves complex interactions that exacerbate tissue deterioration over time. The table below highlights key biomarkers and effects of cellular senescence:
| Biomarkers | Inflammatory Factors | Consequences |
|---|---|---|
| Shortened telomeres | IL-6, IL-1β, TNF-α | Tissue damage |
| p16INK4a expression | SASP components | Chronic inflammation |
| SA-β-gal activity | Pro-inflammatory cytokines | Functional decline |
| DNA damage markers | Cytokine secretion levels | Accelerated aging |
| Mitochondrial dysfunction | SASP-related signaling | Increased tissue stress |
Additionally, understanding the biomarkers of cellular senescence can help in developing strategies to mitigate inflammaging. Recognizing the role of inflammation in aging processes is essential for advancing anti-aging interventions.
Immune Cell Alterations
Aging causes immune cells to undergo significant alterations that drive inflammaging. Cellular senescence accumulates in immune cells, causing them to secrete pro-inflammatory cytokines like IL-6 and TNF-α, fueling chronic inflammation. Comfort solutions for sofa beds and other supportive measures can help improve quality of life, which is crucial as immune function declines with age. Immunosenescence leads to a decline in naive T cells and an increase in exhausted memory T cells, weakening immune responses and promoting persistent low-grade inflammation. Hematopoietic stem cells (HSCs) shift toward myeloid lineages, heightening systemic inflammation. Macrophages and neutrophils show reduced phagocytic and migratory functions, yet produce more inflammatory cytokines. These immune cell alterations disrupt signaling pathways, such as IL-1, IL-6, and TNF-α, further perpetuating inflammaging. Additionally, immune cell aging contributes to the immune regulation imbalance, exacerbating inflammatory responses associated with aging. Moreover, changes in immune signaling pathways can amplify inflammatory processes, worsening age-related health issues. Notably, the accumulation of cellular damage further impairs immune cell function and accelerates inflammaging.
The Role of Immune Cells in Aging-Related Inflammation

As you explore aging-related inflammation, you’ll notice that T cells and B cells become less effective, reducing immune defense and contributing to chronic inflammation. Macrophages also lose their proper function, releasing more inflammatory signals and fueling systemic issues. These immune cell changes play a vital role in the persistent, low-grade inflammation linked to aging. Additionally, beetroot-rich diets may help support immune health by providing essential nutrients that promote proper immune cell function.
Decline in T Cells
The decline in T cell function is a key factor driving inflammation associated with aging. As you age, your immune system produces fewer naive T cells, limiting your ability to respond to new infections.
Meanwhile, senescent T cells accumulate, secreting pro-inflammatory cytokines that fuel inflammaging. This process reduces immune diversity and hampers pathogen recognition.
Specifically:
- The buildup of senescent T cells worsens systemic inflammation by releasing cytokines that promote chronic inflammation.
- Reduced TCR diversity impairs the immune system’s capacity to combat novel pathogens effectively.
- Dysfunctional T cells exhibit mitochondrial and epigenetic abnormalities, further increasing inflammatory signaling.
Additionally, research indicates that immune cell decline plays a central role in the development of chronic inflammation in aging populations.
Together, these changes weaken your immune defenses and contribute to the persistent inflammation characteristic of aging.
B Cell Exhaustion
B cell exhaustion plays a significant role in driving inflammation associated with aging by impairing humoral immunity.
As you age, your immune system experiences a decline in B cell lymphopoiesis, leading to fewer new B cells and weaker antibody responses. The peripheral B cell pool shifts toward exhausted memory B cells, which produce fewer effective antibodies and generate more autoantibodies.
Reduced IL-7 levels diminish B cell precursors and plasma cell formation in the bone marrow, further weakening immune defenses.
The accumulation of senescent B cells with SASP features promotes inflamm-aging by releasing pro-inflammatory factors, fueling systemic inflammation.
This process hampers your immune response, increases susceptibility to infections, and sustains the chronic inflammatory state characteristic of aging.
Macrophage Function Loss
Aging impairs macrophage function, reducing their ability to detect and eliminate pathogens effectively. This decline contributes to inflammaging, a chronic, low-grade inflammation linked to age-related diseases. Dysfunctional macrophages secrete more pro-inflammatory cytokines like TNF-α, IL-6, and IL-1β, fueling systemic inflammation.
Additionally, impaired mitochondrial calcium signaling causes persistent activation of these cells, worsening tissue damage. To understand this better:
- Macrophages become less responsive to stimuli, weakening immune defenses.
- Increased cytokine secretion promotes a pro-inflammatory environment.
- Loss of mitochondrial calcium regulation sustains inflammaging.
Signaling Pathways That Fuel Inflammaging

Multiple signaling pathways drive inflammaging by amplifying and sustaining chronic low-grade inflammation. The NF-κB pathway plays a central role, activating genes that produce cytokines like IL-1, IL-6, and TNF-α, fueling ongoing inflammation.
Senescent cells release SASP factors that further engage NF-κB, creating a feedback loop.
Mitochondrial dysfunction increases reactive oxygen species (ROS), which activate inflammasomes—multiprotein complexes that promote the release of pro-inflammatory cytokines.
Excess ROS also damages cellular components, maintaining inflammatory signals.
Disrupted autophagy impairs the clearance of damaged mitochondria and proteins, perpetuating these pathways.
Organ-Level Effects of Persistent Inflammation

Persistent inflammation driven by signaling pathways like NF-κB and mitochondrial dysfunction directly damages organ tissues, leading to functional decline. Chronic inflammation impairs the organ’s regenerative capacity, causing tissue fibrosis and cellular senescence that accelerate aging.
Elevated cytokines such as IL-6 and TNF-α sustain local inflammation, worsening tissue remodeling. Microvascular damage reduces blood flow, further impairing organ function.
Consider these points:
- Cellular senescence and SASP factors foster a pro-inflammatory environment, compounding tissue damage.
- Tissue fibrosis replaces healthy tissue with scar-like material, diminishing organ performance.
- Microvascular damage leads to decreased blood supply, heightening vulnerability to age-related diseases.
Together, these effects contribute to organ dysfunction, heightening susceptibility to chronic illnesses in aging.
Molecular Biomarkers of Inflammaging

Molecular biomarkers of inflammaging provide essential insights into the aging process by reflecting underlying cellular and systemic changes. You can measure biomarkers like cytokines—such as IL-6, IL-1β, and TNF-α—that increase with age, indicating chronic low-grade inflammation.
Elevated levels of circulating C-reactive protein (CRP) also serve as systemic markers linked to aging-related health decline. The presence of senescent cells, identified through biomarkers like p16^INK4a^ and SA-β-gal, signifies heightened inflammaging.
Additionally, gene expression patterns in immune cells reveal transcriptomic and epigenetic signatures associated with aging. These molecular biomarkers allow you to track cellular senescence, inflammatory activity, and systemic changes, providing a thorough picture of inflammaging and its role in the aging process.
Strategies to Counteract Inflammaging Naturally and Clinically
You can actively combat inflammaging by adopting lifestyle strategies that reduce inflammation and support healthier aging. These approaches modulate the inflammatory response and promote anti-inflammatory cytokine production, slowing the aging process.
- Follow an anti-inflammatory diet rich in fruits, leafy greens, fatty fish, nuts, and whole grains to combat systemic inflammation.
- Engage in regular physical activity like walking or swimming to lower inflammatory markers such as IL-6 and TNF-alpha.
- Manage stress through techniques like meditation and quit smoking to decrease chronic inflammation and support healthier aging.
Implementing these habits helps maintain immune balance, reduces chronic inflammation, and fosters a more resilient aging process, ultimately promoting longevity and well-being.
Emerging Technologies and Therapies for Age-Related Inflammation

Emerging technologies like senolytics are designed to target senescent cells and reduce inflammation linked to aging.
Advances in single-cell analysis allow you to identify inflammatory pathways and immune cell changes with high precision.
Meanwhile, new therapies aim to modulate cytokines and restore mitochondrial function to combat inflammaging effectively.
Senolytics Targeting Senescent Cells
Have you ever wondered how scientists are tackling the root causes of age-related inflammation? They’re developing senolytics—drugs that target and eliminate senescent cells, which secrete pro-inflammatory factors known as SASP. Removing these cells reduces chronic inflammation and improves tissue health.
Here are three key points to understand:
- Senolytics like Dasatinib and Quercetin selectively remove senescent cells, decreasing SASP-related inflammation.
- Clearing these cells has shown promising results in mice, improving tissue function and extending lifespan.
- Ongoing clinical trials aim to confirm the safety and effectiveness of senolytics for treating age-related inflammation in humans.
Immune Modulation Strategies
To combat age-related inflammation, scientists are developing innovative immune modulation strategies that target the underlying immune system changes associated with aging. These include senolytics like Dasatinib and Quercetin, which selectively eliminate senescent cells that secrete pro-inflammatory cytokines. New drugs aim to modulate cytokines such as IL-6, IL-1, and TNF-alpha, reducing chronic inflammation. Additionally, enhancing autophagy restores cellular cleanup processes, mitigating inflammaging. Advanced technologies like single-cell analysis enable detailed profiling of immune cell changes, fostering personalized therapies. Here’s a quick overview:
| Strategy | Focus Area |
|---|---|
| Senolytics | Clearing senescent cells |
| Cytokine Inhibitors | Modulating inflammatory signals |
| Autophagy Enhancement | Improving cellular health |
Single-Cell Analysis Advances
Single-cell analysis technologies, such as single-cell RNA sequencing, are revolutionizing our understanding of age-related inflammation by allowing you to examine individual immune cells with unmatched detail. These tools reveal cellular heterogeneity, helping you identify pro-inflammatory cytokine-producing cells driving inflammaging.
By analyzing immune cells at the single-cell level, researchers uncover specific molecular pathways responsible for chronic inflammation in aging tissues.
- Pinpoint distinct immune cell subsets linked to inflammation.
- Discover biomarkers for early detection of inflammaging.
- Develop targeted therapies to modulate immune cell functions.
This approach enables precise mapping of cellular states, offering new possibilities for personalized interventions in age-associated inflammatory diseases. Single-cell analysis fundamentally enhances our ability to understand and combat inflammaging.
Lifestyle Modifications to Reduce Inflammaging and Promote Healthy Aging

Adopting healthy lifestyle habits is essential for reducing inflammaging and supporting healthy aging. Your lifestyle choices directly influence your immune system and inflammatory responses.
An anti-inflammatory diet rich in fruits, leafy greens, fatty fish, nuts, olive oil, and whole grains can lower chronic inflammation.
Regular physical activity, like walking or swimming, helps decrease inflammatory markers linked to aging.
Quitting smoking and avoiding processed foods, refined carbs, and fried items reduce pro-inflammatory cytokines, promoting better immune health.
Managing stress through meditation and getting enough sleep are critical strategies to combat inflammaging.
Additionally, maintaining a healthy weight and engaging in strength training or stretching enhances your body’s anti-inflammatory capacity, supporting overall longevity and vitality as you age.
Frequently Asked Questions
What Is the Inflammatory Theory of Ageing?
You might wonder what drives aging, and the inflammatory theory suggests it’s chronic, low-grade inflammation.
As you age, your immune system produces more pro-inflammatory molecules like IL-6, TNF-α, and IL-1, leading to systemic inflammation.
This process is fueled by cellular aging and damaged cells, creating a cycle that accelerates aging.
Managing this inflammation through healthy lifestyle choices could help slow down the aging process and related health issues.
Is Inflammaging the Same as Inflammation?
You might wonder if inflammaging is the same as inflammation. While both involve immune responses, inflammaging is a specific, chronic, low-grade inflammation that develops gradually with age.
Unlike typical inflammation, which reacts to injury or infection and resolves quickly, inflammaging persists without clear cause, contributing to tissue damage and age-related diseases.
How Is Inflammation Linked to Aging?
So, you’re wondering how inflammation links to aging? Well, as you get older, your body starts acting like a cranky old timer, constantly simmering with low-grade inflammation. This persistent fuss, driven by cellular senescence and immune decline, speeds up aging and invites age-related diseases like Alzheimer’s and arthritis.
Fundamentally, your body’s internal fireworks are firing off more often, making aging feel like a never-ending party you didn’t RSVP to.
What Is the Main Cause of Inflammation in the Body?
The main cause of inflammation in your body as you age is the dysfunction of mitochondria in your immune cells, especially macrophages.
As mitochondria struggle to regulate calcium properly, they produce excess reactive oxygen species that damage cells and trigger inflammation.
This process worsens when your body’s ability to clear out damaged mitochondria declines, leading to a constant, low-grade inflammation known as inflammaging that accelerates aging and health decline.
What Contributes to Inflammaging?
You might think inflammation naturally slows down as you age, but actually, it builds up due to your body’s changing cells.
Senescent cells release harmful SASP factors, while damaged mitochondria and increased oxidative stress add to the problem.
Disrupted signaling pathways and altered calcium levels in immune cells keep inflammation persistent.
This combination creates a cycle that leads to chronic, low-grade inflammation—what we call inflammaging—making aging more complex than it seems.
Conclusion
By understanding inflammaging, you can see it as a slow-burning fire inside, gradually fueling aging and disease. Embracing lifestyle changes, innovative therapies, and early detection can help extinguish this blaze before it consumes your health. Think of it as tending a garden—regular care keeps the weeds of inflammation at bay, allowing your body to thrive in the golden years. Take action now, and nurture your journey toward healthier, more vibrant aging.









